Hernia Surgery
Skip the waiting list – book your NHS hernia repair surgery with Independent Health Group for a low-risk, hassle-free procedure.

Short waiting time

Recommended by 99% of our patients

What is a hernia?
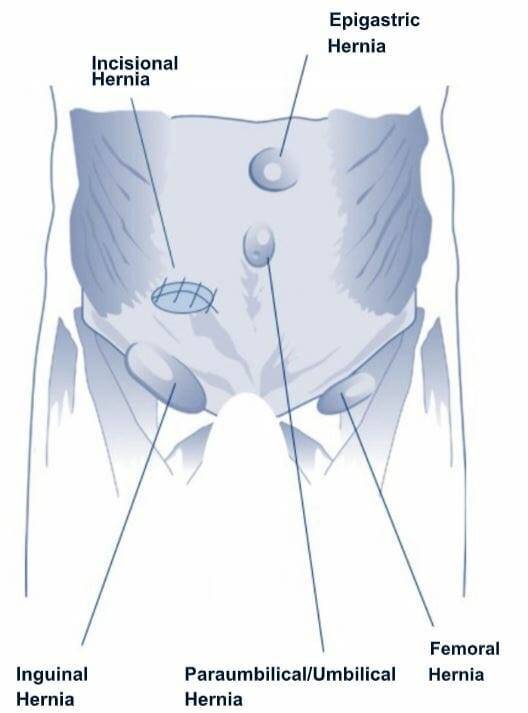
A hernia is caused when an internal organ or tissue within the abdominal cavity pushes through a weakened area of the abdominal wall. This typically occurs in either the abdomen or groin area and results in a noticeable swelling or bulge.
Hernias are a common condition that affects men more commonly than women. They tend to manifest quite suddenly and are known to commonly appear after performing strenuous physical activity.
They can also be incredibly discomforting and come in various forms, each associated with various locations within the body. Some of the most common types of hernia include:
- Inguinal hernia – the most common type of hernia that develops on either side of the groin, typically caused when a portion of the intestine protrudes into the inguinal canal.
- Femoral hernia – more common in women than men, this type of hernia occurs when an organ or tissue pushes through the femoral canal, a passageway located near the upper thigh.
- Incisional hernia – this hernia develops at the site of an incision or scar, where the abdominal wall has previously been weakened as a result of surgery.
Do you need hernia surgery?

Why book your hernia surgery with the Independent Health Group?
Here at Independent Health Group, we are proud to provide high-quality NHS treatments to local patients throughout England.
Our unique community-centred structure allows us to offer NHS patients faster access to vital healthcare from a more convenient location at no extra cost. This includes all types of hernia repair surgery – from keyhole hernia surgery to umbilical hernia surgery – and allows you to avoid the long waiting lists typically found at larger hospitals.
Offering state-of-the-art equipment, we have facilities throughout the UK, with each one comprised of a specialist team of friendly staff and highly experienced surgeons.
Following an initial consultation with us, we will aim to provide you with a date for your hernia surgery within 11 weeks. We will also ensure you work with the same clinician throughout, offering you some added peace of mind throughout your treatment journey.

What our patients say
Excellent communication and care from start to finish
Aspen Centre – Apr 24
No big wait time, straight in and welcomed into surgery
The County Practice, Syston – Apr 24
Great care from all of the nurses and doctors
Aspen Centre – Mar 24
I felt immediately relaxed by all the friendly staff who executed confidence
The County Practice, Syston – Mar 24
Brilliant. Hernia detected and fixed in 2 weeks! Surgery done very competently, without significant pain
Aspen Centre – Jan 24
Brilliant surgeon and team. Friendly, caring, and chatty. Well done <3 x
The County Practice, Syston – Jan 24
Made to feel relaxed and supported through procedure.
Aspen Centre – Nov 23
Well organised, well informed, friendly and professional.
The County Practice, Syston – Nov 23
I felt looked after and cared for all the way through pre-surgery and surgery.
Aspen Centre – Oct 23
The staff were friendly and well aware of my needs and therefore kept me suitably distracted.
The County Practice, Syston – Oct 23
Fantastic care, and excellent service.
Aspen Centre – Sept 23
Everyone I met today was excellent. Very friendly and attentive.
The County Practice, Syston – Sept 23
Get in touch

